I remember the first time I Googled the word “zit”. I was 14, and my skin had just begun breaking out (much to my insecure, adolescent delight). Naturally, I wanted to learn more. I wanted to figure out what was going on, and what I could do about it.
Researching zits—as I quickly found out—isn’t straightforward as you might think. The words are long, the science is confusing, and the advice often contradicts itself. Sure, some of what you read makes sense; like that zits can be caused by stress or hormones, and you probably shouldn’t pick at one. But then you enter a territory where things get a little confusing, with terminology that creates more questions than answers.
And this seems to be shared by a lot of people. If you look into hyperpigmentation to try and figure it out, you’re given a lot of conflicting information on how it's caused and how best to treat it. It’s confusing, and understandably so because hyperpigmentation is a broad condition.
To put it simply, hyperpigmentation is the process through which areas of your skin become a darker shade. Some people propose that hyperpigmentation is a form of scarring, which is actually wrong. It’s an increase in melanin production.
In your skin, you have cells called 'melanocytes', and their job is to produce melanin, the body’s natural defense against UV, and the reason your skin has color natural pigment. On a normal day, the melanocytes remained composed, and the production of your melanin, which is known as 'melanogenesis' remains calm, cool and composed. But what can happen is that some of those melanocytes can be stimulated to a point where they produce more melanin than normal.
This is where it becomes a little confusing because there’s more than one why. For example, hyperpigmentation can come from increased exposure to the sun, with increased melanin being a form of safety mechanism. But then you have conditions like melasma—a form of hyperpigmentation that’s a result of a fluctuation in hormones such as estrogen or progesterone—inducing the production of melanin. In fact, a person can develop hyperpigmentation from smoking (another reason not to), from having tinea, or whilst she is pregnant. And then you have post-inflammation hyperpigmentation, which is where zits come into the picture.

When your skin gets a cut or a burn or an abrasion, and your body detects an infection of microorganisms, your immune system responds by flooding that area with white blood cells. That's what inflammation is. It’s the same for when bacteria starts building when a pore becomes blocked.
When a part of your skin becomes inflamed, the process can have an inadvertent reaction to your skin cells, particularly your melanocytes and the stimulation melanogenesis.
That’s precisely why so many experts warn against the risk of hyperpigmentation when it comes to scratching or popping zits: Your body’s natural healing response may leave you with something that sticks around for longer than you’d like. But what if we told you we knew a way to fast-forward hyperpigmentation? ⏩
You wouldn't sit through a movie that sucks. So why are you waiting for post-zit damage to fade on its own? There's a faster way, down below.
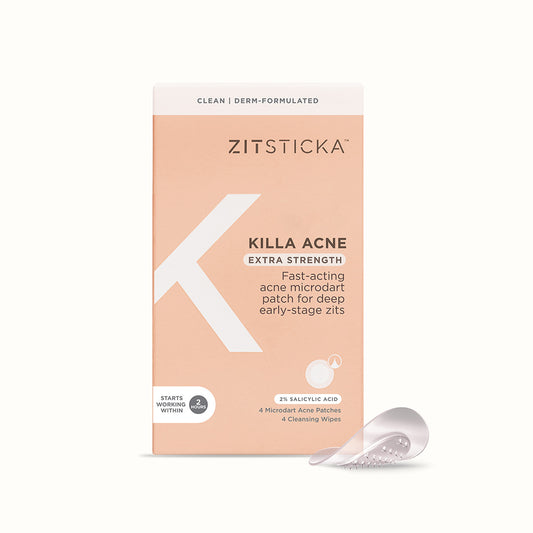
Shop HYPERFADE, a microdart patch for dark spots.
Images: @annamariereilly, @beauty4brownskin